What Are The Key Causes Of Bunions?
Overview
Sometimes, the big toe can become angled outwards towards the middle of the foot and second toe. This forces the top of the first metatarsal to stick out from the side of the foot at the base of the big toe. If this happens, the bones can become misaligned and a painful bunion can form. It is not known exactly what causes bunions, but wearing badly fitting shoes is thought to make the condition worse. Research also suggests that bunions may run in families. It is thought that bunions are more likely to occur in people who have unusually flexible joints, and that this flexibility may be inherited. In some cases, certain health conditions, such as rheumatoid arthritis and gout, may also be responsible for the formation of bunions. These conditions cause pain and inflammation in the joints.
Causes
Bunions can be caused by improper footwear. Genetics. Foot injuries. Congenital deformities. Medical conditions such as arthritis. Stress on feet. Bunions are mainly caused by genetics. The bunion itself is not inherited, but the person?s hereditary foot type and gait pattern makes them more prone to developing bunions.You can also begin to develop bunionsby wearing shoes that are too tight or too small. When you wear shoes of this nature, your toes are squeezed together. Bunions are not caused by crowding of the toes, but wearing tight shoes can worsen the condition and cause symptoms to appear sooner. Some people are born with birth defects that put them at higher risk for developing bunions.
Symptoms
Bunions or hallux valgus tend to give pain predominantly from the metatarsal head on the inner border of the foot. The bunion tends to be painful mainly when in enclosed shoes and so is often more symptomatic in winter. As the front part of the foot splays and the great toe moves across towards the 2nd toe a bunion can also produce pain from the 2nd toe itself. The pain which a bunion produces on the 2nd toe is either due to direct rubbing between the great toe and the 2nd toe, a hammer toe type deformity produced due to crowding of the 2nd toe by the bunion and the 3rd toe.The hammer toe will either be painful from its top aspect where it rubs directly on shoe wear or its under surface in the area of the 2nd metatarsal head. This is made prominent and pushed to the sole of the foot by the 2nd toe rising upwards and driving the metatarsal head downwards.
Diagnosis
A doctor can very often diagnose a bunion by looking at it. A foot x-ray can show an abnormal angle between the big toe and the foot. In some cases, arthritis may also be seen.
Non Surgical Treatment
Bunions can develop at any time. Although bunions often require no medical treatment you should consult your family doctor/chiropodist/podiatrist. Treatment options vary depending on the severity of your bunion and the amount of pain it causes you. Although they don't always cause problems, bunions are permanent unless surgically corrected. If the cushioning sac of fluid (bursa) over the affected joint becomes inflamed (bursitis), a bunion can be very painful and interfere with your normal activities. Bunions may get larger and more painful, making nonsurgical treatment less effective. Apply a non-medicated bunion pad around the bony bump. If a bunion becomes inflamed or painful, apply an ice pack two to three times daily to help reduce swelling. Wear shoes with a wide and deep toe box. Avoid shoes with heels higher than 2 inches (5.1 centimeters). 
Surgical Treatment
There is more than one way to surgically treat a bunion. While there are some general guidelines, some procedures work well for some Surgeons and poorly for others. Your Surgeon should consider the severity of your bunion, medical condition, lifestyle, and recuperation time when considering the surgical treatment.
Prevention
If you are genetically at risk, not a lot. But shoes that are too narrow, too tight (even ballet flats) or have very high heels that force your toes down into the pointed end are asking for trouble. Aim for a 1cm gap between your toes and the end of your shoes. This doesn?t mean wearing frumpy flatties, the Society of Podiatrists and Chiropodists recommends sticking to 4cm heels for everyday wear, and wearing different types of shoe to vary the position of your foot. Gladiator styles can help because the straps stop your foot pushing down into the point of the shoe, ditto Mary Janes (sorry but for beautiful feet they need to have a strap), and flat, wide-fitting brogues are a no-brainer. Alternatively, in summer you can wear flip-flops to keep the space between your big and second toe as wide as possible. If you have children it?s vital to make sure that their feet are measured for properly fitting shoes to nip any potential problems in the bud. Keeping your feet and lower legs supple and strong is important too, that?s how A-list celebs get away with wearing killer heels, they all work-out like crazy. Exercises like trying to widen the space between your big toe and the second one with your foot flat on the floor, a few times a day can help, as can calf stretches. If you are devoted to any exercise that involves high impact for your feet, it might be worth checking that your gait and shoes are correct with a specialist shop such as Runners Need, as poor styles can cause irreparable bunion-related problems that will consign your trainers to the back of the cupboard for ever.
Overpronation Of The Feet
Overpronation is a term that gets thrown around a lot by psuedo-experts and there is so much written online about it, that it can get very confusing to determine what is legitimate and what is not. Pronation is a normal motion of the foot that occurs when the ankle rolls inwards and the arch collapses. This is normal. Its not something evil. Overpronation is assumed to be when there is too much of it. There certainly is debate as to just how much is too much, as some people have large amounts and have no problems, other have small amounts and do have problems. It all comes down to individual differences and how much force is needed to stop the foot moving. The greater the force, regardless of the amounts of pronation, the more likely it is to be a problem. Some still like to debate if it is a problem or not. Some studies have shown that its not a problem and other studies have shown it is. If the data from all these studies are pooled, then the conclusion was that, yes, overpronation is a problem that was statistically significant, but it was only a small risk factor for problems. An associated finding of overpronation during a gait analysis is an abductory twist.

Causes
There are many biomechanical issues that can contribute to excessive pronation, including weak foot intrinsic muscles, limited ankle dorsiflexion mobility and calf flexibility, weak ankle invertor muscles (e.g. posterior tibialis), weak forefoot evertor muscles (peroneus longus), poor hip strength and control, Anterior pelvic tilting, heel InversionIn a person who overpronates, the heel bone goes into an everted position meaning that it turns out away from the midline of the body. The opposite motion of eversion is inversion. Inversion is a motion that needs to be controlled to prevent the foot from excessively pronating.
Symptoms
Symptoms can manifest in many different ways. Here is a list of some of the common conditions associated with over-pronation in children. Achilles Pain. Ankle pain. Arch Pain. Low back pain. Heel Pain. Knee Pain (Runner's knee and Chondromalecia of the patella) Osgood Schlatter Disease (pain below the knee) Shin Splints (pain in the front of the lower leg) Over-pronation does not necessarily mean your child has "flat feet." Even though children's arches may be relatively high when they lie down or sit, over-pronation may not be seen until your child is standing. A certain amount of pronation is normal. During normal walking or running ("gait cycle"), the heel strikes the ground and the foot rolls inward to absorb shock and adapt to the surface. This gait cycle is even more important if the running surface is uneven.
Diagnosis
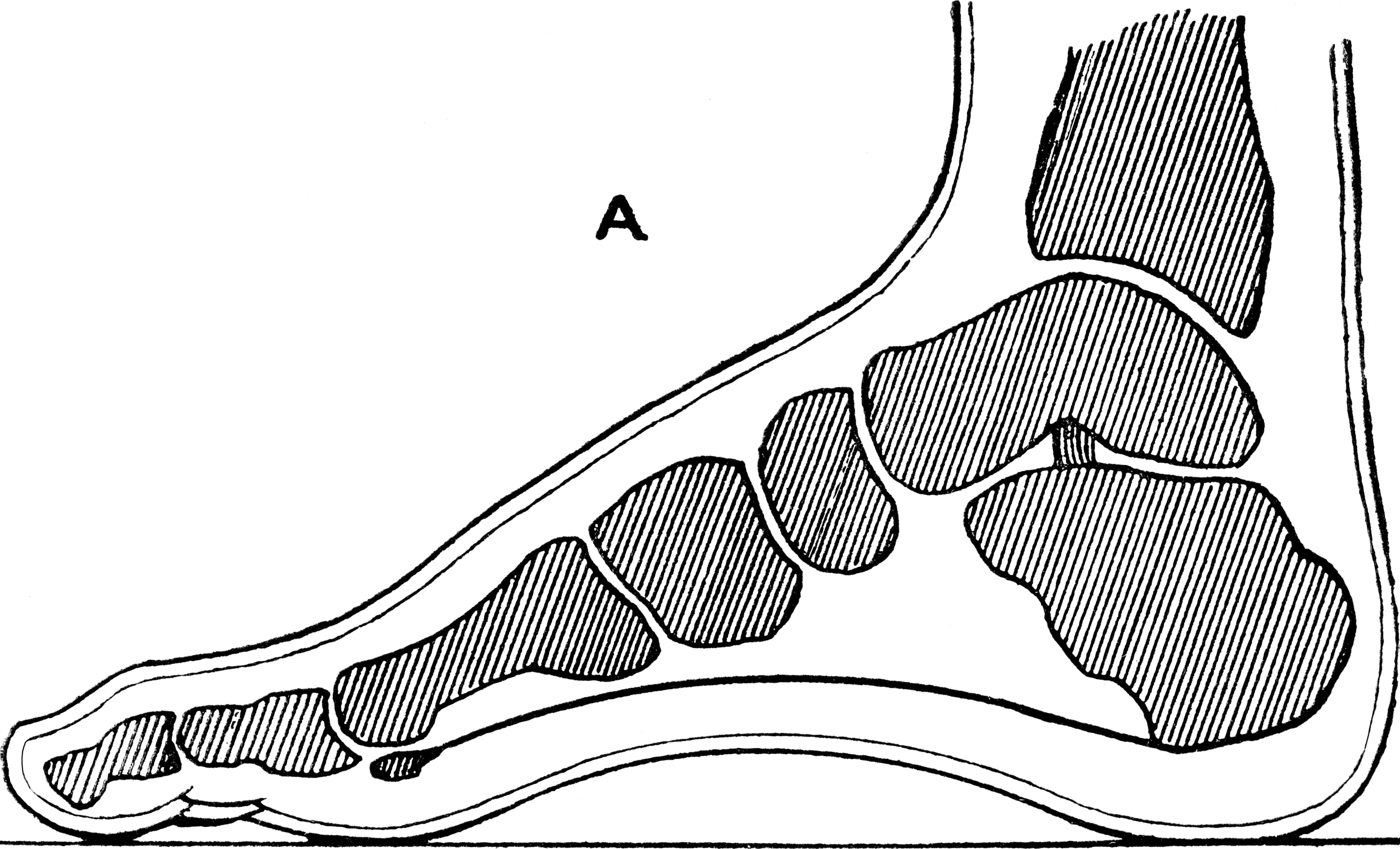
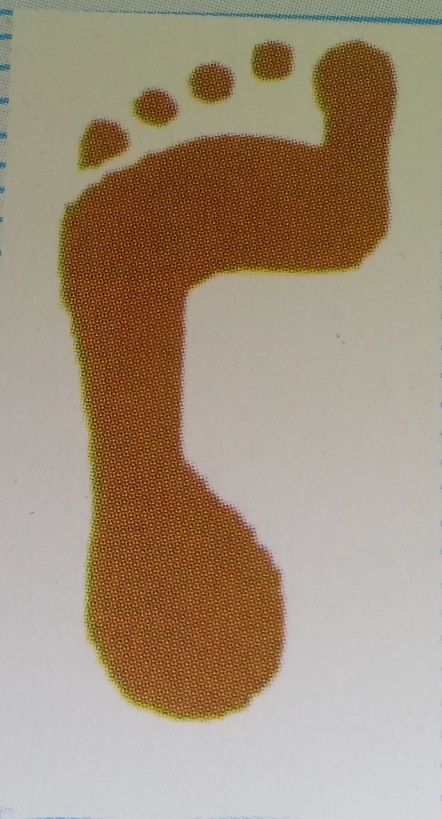
Firstly, look at your feet in standing, have you got a clear arch on the inside of the foot? If there is not an arch and the innermost part of the sole touches the floor, then your feet are over-pronated. Secondly, look at your running shoes. If they are worn on the inside of the sole in particular, then pronation may be a problem for you. Thirdly, try the wet foot test. Wet your feet and walk along a section of paving and look at the footprints you leave. A normal foot will leave a print of the heel, connected to the forefoot by a strip approximately half the width of the foot on the outside of the sole. If you?re feet are pronated there may be little distinction between the rear and forefoot, shown opposite. The best way to determine if you over pronate is to visit a podiatrist or similar who can do a full gait analysis on a treadmill or using forceplates measuring exactly the forces and angles of the foot whilst running. It is not only the amount of over pronation which is important but the timing of it during the gait cycle as well that needs to be assessed.
Non Surgical Treatment
An orthotic is a device inserted inside the shoe to assist in prevention and/or rehabilitation of injury. Orthotics support the arch, prevent or correct functional deformities, and improve biomechanics. Prescription foot orthoses are foot orthoses which are fabricated utilizing a three dimensional representation of the plantar foot and are specifically constructed for an individual using both weightbearing and nonweightbearing measurement parameters and using the observation of the foot and lower extremity functioning during weightbearing activities. Non-prescription foot orthoses are foot which are fabricated in average sizes and shapes in an attempt to match the most prevalent sizes and shapes of feet within the population without utilizing a three dimensional representation of the plantar foot of the individual receiving the orthosis.
Prevention
Many of the prevention methods for overpronation-orthotics, for example-can be used interchangeably with treatment methods. If the overpronation is severe, you should seek medical attention from a podiatrist who can cast you for custom-made orthotics. Custom-made orthotics are more expensive, but they last longer and provide support, stability, and balance for the entire foot. You can also talk with a shoe specialist about running shoes that offer extra medial support and firm heel counters. Proper shoes can improve symptoms quickly and prevent them from recurring. Surgery can sometimes help cure and prevent this problem if you suffer from inherited or acquired pes planus deformity. Surgery typically involves stabilizing the bones to improve the foot?s support and function.
Severs Disease The Facts
Pain in the heel of a child's foot, typically brought on by some form of injury or trauma, is sometimes Sever's Disease. The disease often mimics Achilles tendonitis, an inflammation of the tendon attached to the back of the heel. A tight Achilles tendon may contribute to Sever's Disease by pulling excessively on the growth plate of the heel bone. This condition is most common in younger children and is frequently seen in the active soccer, football or baseball player. Sport shoes with cleats are also known to aggravate the condition. Treatment includes calf muscle stretching exercises, heel cushions in the shoes, and/or anti-inflammatory medications. Consult your physician before taking any medications.
Causes
Your child is most at risk for this condition when he or she is in the early part of the growth spurt in early puberty. Sever's disease is most common in physically active girls 8 years to 10 years of age and in physically active boys 10 years to 12 years of age. Soccer players and gymnasts often get Sever's disease, but children who do any running or jumping activity may also be at an increased risk. Sever's disease rarely occurs in older teenagers because the back of the heel has typically finished growing by 15 years of age.
Symptoms
Symptoms include Heel Pain. Pain at the back of the heels when walking or running. Possibly a lump at the back of the heel, although this might be minimal. Pain and tenderness at the back of the heels, especially if you press on it, or give it a squeeze from the sides. Tight calf muscles resulting in reduced ankle range of motion.
Diagnosis
Children or adolescents who are experiencing pain and discomfort in their feet should be evaluated by a physician. In some cases, no imaging tests are needed to diagnose Sever?s disease. A podiatrist or other healthcare professional may choose to order an x-ray or imaging study, however, to ensure that there is no other cause for the pain, such as a fracture. Sever?s disease will not show any findings on an x-ray because it affects cartilage.
Non Surgical Treatment
Occasionally, an orthotic may need to be prescribed for temporary or long-term correction of their foot biomechanics (eg flat feet or high arches). During the acute phase of Sever's disease a small heel rise or shock-absorbing heel cup placed under the heel pad of your child's foot may help to ease the symptoms. Your podiatrist or physiotherapist can assess your child's arch and guide you in the best management of your child's condition. We recommend that your child should never go barefooted during the painful stages of Sever's disease.
Recovery
This condition is self limiting, it will go away when the two parts of bony growth join together, this is natural. Unfortunately, Sever's disease can be very painful and limit sport activity of the child while waiting for it to go away, so treatment is often advised to help relieve it. In a few cases of Sever's disease, the treatment is not successful and these children will be restricted in their activity levels until the two growth areas join, usually around the age of 16 years. There are no known long term complications associated with Sever's disease.
Treatments And Causes
Overview
Flatfoot deformity is a general term used to describe a person whose arches are slowly dropping to the ground, aka ?fallen arches.? Adult-acquired flatfoot deformity can be caused by several factors, but the most common is abnormal functioning of the posterior tibial tendon in the foot and ankle. The posterior tibial tendon is the primary tendon that supports the arch. If this tendon begins to elongate from a sustained, gradual stretch over a long period of time, then the arch will progressively decrease until full collapse of the arch is noted on standing. What makes this tendon elongated? Biomechanical instability of the foot such as over-pronation or an accessory bone at the insertion site of the tendon are the primary causes for posterior tibial tendon dysfunction. 
Causes
Adult flatfoot typically occurs very gradually. If often develops in an obese person who already has somewhat flat feet. As the person ages, the tendons and ligaments that support the foot begin to lose their strength and elasticity.
Symptoms
Symptoms are minor and may go unnoticed, Pain dominates, rather than deformity. Minor swelling may be visible along the course of the tendon. Pain and swelling along the course of the tendon. Visible decrease in arch height. Aduction of the forefoot on rearfoot. Subluxed tali and navicular joints. Deformation at this point is still flexible. Considerable deformity and weakness. Significant pain. Arthritic changes in the tarsal joints. Deformation at this point is rigid.
Diagnosis
Starting from the knee down, check for any bowing of the tibia. A tibial varum will cause increased medial stress on the foot and ankle. This is essential to consider in surgical planning. Check the gastrocnemius muscle and Achilles complex via a straight and bent knee check for equinus. If the range of motion improves to at least neutral with bent knee testing of the Achilles complex, one may consider a gastrocnemius recession. If the Achilles complex is still tight with bent knee testing, an Achilles lengthening may be necessary. Check the posterior tibial muscle along its entire course. Palpate the muscle and observe the tendon for strength with a plantarflexion and inversion stress test. Check the flexor muscles for strength in order to see if an adequate transfer tendon is available. Check the anterior tibial tendon for size and strength.
Non surgical Treatment
Conservative treatment is indicated for nearly all patients initially before surgical management is considered. The key factors in determining appropriate treatment are whether acute inflammation and whether the foot deformity is flexible or fixed. However, the ultimate treatment is often determined by the patients, most of whom are women aged 40 or older. Compliance can be a problem, especially in stages I and II. It helps to emphasise to the patients that tibialis posterior dysfunction is a progressive and chronic condition and that several fittings and a trial of several different orthoses or treatments are often needed before a tolerable treatment is found. 
Surgical Treatment
Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
Adult Aquired Flat Foot (AAF) What Exactly Is It
Adult acquired flatfoot deformity (AAFD) is a painful, chronic condition found most often in women between the ages of 40 and 60. AAFD occurs when the soft tissues of the foot are overstretched and torn, causing the arch to collapse. Flatfoot deformities may also be caused by a foot fracture, or may result from long-term arthritis. Once the posterior tibial tendon-the tendon unit that holds up the arch-loses its function, the foot becomes flat as the bones spread out of position during weight bearing. Without an AAFD repair, the condition may progress until the affected foot becomes entirely rigid and quite painful.
Causes
There are multiple factors contributing to the development of this problem. Damage to the nerves, ligaments, and/or tendons of the foot can cause subluxation (partial dislocation) of the subtalar or talonavicular joints. Bone fracture is a possible cause. The resulting joint deformity from any of these problems can lead to adult-acquired flatfoot deformity. Dysfunction of the posterior tibial tendon has always been linked with adult-acquired flatfoot deformity (AAFD). The loss of active and passive pull of the tendon alters the normal biomechanics of the foot and ankle. The reasons for this can be many and varied as well. Diabetes, high blood pressure, and prolonged use of steroids are some of the more common causes of adult-acquired flatfoot deformity (AAFD) brought on by impairment of the posterior tibialis tendon. Overstretching or rupture of the tendon results in tendon and muscle imbalance in the foot leading to adult-acquired flatfoot deformity (AAFD). Rheumatoid arthritis is one of the more common causes. About half of all adults with this type of arthritis will develop adult flatfoot deformity over time. In such cases, the condition is gradual and progressive. Obesity has been linked with this condition. Loss of blood supply for any reason in the area of the posterior tibialis tendon is another factor. Other possible causes include bone fracture or dislocation, a torn or stretched tendon, or a neurologic condition causing weakness.
Symptoms
Initially, flatfoot deformity may not present with any symptoms. However, overtime as the tendon continues to function in an abnormal position, people with fallen arches will begin to have throbbing or sharp pain along the inside of the arch. Once the tendon and soft tissue around it elongates, there is no strengthening exercises or mechanism to shorten the tendon back to a normal position. Flatfoot can also occur in one or both feet. If the arch starts to slowly collapse in one foot and not the other, posterior tibial dysfunction (PTTD) is the most likely cause. People with flatfoot may only have pain with certain activities such as running or exercise in the early phase of PTTD. Pain may start from the arch and continue towards the inside part of the foot and ankle where the tendon courses from the leg. Redness, swelling and increased warmth may also occur. Later signs of PTTD include pain on the outside of the foot from the arch collapsing and impinging other joints. Arthritic symptoms such as painful, swollen joints in the foot and ankle may occur later as well due to the increased stress on the joints from working in an abnormal position for a long period of time.
Diagnosis
Diagnostic testing is often used to diagnose the condition and help determine the stage of the disease. The most common test done in the office setting are weightbearing X-rays of the foot and ankle. These assess joint alignment and osteoarthritis. If tendon tearing or rupture is suspected, the gold standard test would be MRI. The MRI is used to check the tendon, surrounding ligament structures and the midfoot and hindfoot joints. An MRI is essential if surgery is being considered.
Non surgical Treatment
Treatment depends very much upon a patient?s symptoms, functional goals, degree and specifics of deformity, and the presence of arthritis. Some patients get better without surgery. Rest and immobilization, orthotics, braces and physical therapy all may be appropriate. With early-stage disease that involves pain along the tendon, immobilization with a boot for a period of time can relieve stress on the tendon and reduce the inflammation and pain. Once these symptoms have resolved, patients are often transitioned into an orthotic that supports the inside aspect of the hindfoot. For patients with more significant deformity, a larger ankle brace may be necessary.

Surgical Treatment
Flatfoot reconstruction (osteotomy). This is often recommended for flexible flatfoot condition. Flatfoot reconstruction involves cutting and shifting the heel bone into a more neutral position, transferring the tendon used to flex the lesser toes (all but the big toe) to strengthen the posterior tibial tendon, and lengthening the calf muscle. Fusion (also known as triple arthrodesis). Fusion involves fusing, or making stiff, three joints in the back of the foot the subtalar, talonavicular, and calcaneocuboid joints, to realign the foot and give it a more natural shape. Pins or screws hold the area in place until it heals. Fusion is often recommended for a rigid flatfoot deformity or evidence of arthritis. Both of these surgeries can provide excellent pain relief and correction.
Coping With Achilles Tendonitis
 Achilles tendinitis is when the tendon that connects the back of your leg to your heel becomes swollen and painful near the bottom of the foot. This tendon is called the Achilles tendon. It is used for walking, running, and jumping.
Achilles tendinitis is when the tendon that connects the back of your leg to your heel becomes swollen and painful near the bottom of the foot. This tendon is called the Achilles tendon. It is used for walking, running, and jumping.
Causes
Most common in middle-aged men. Conditions affecting the foot structure (such as fallen arches). Running on uneven, hilly ground, or in poor quality shoes. Diabetes. High blood pressure. Certain antibiotics. ?Weekend Warriors?. Recent increase in the intensity of an exercise program. While Achilles tendinitis can flare up with any overuse or strain of the Achilles tendon, it most often affects middle-aged men, especially if they are ?weekend warriors? who are relatively sedentary during the week, then decide to play basketball or football on Saturday. Those with flat feet or other structural conditions affecting their feet tend to put excess strain on the Achilles tendon, increasing their chances of developing Achilles tendinitis or even rupturing the tendon. If you are a runner, be sure to only run in quality running shoes that are supportive and well cushioned, and to be mindful of the surface you?re running on. Uneven surfaces and especially hilly terrain put additional strain on your Achilles tendon and can lead to the condition.
Symptoms
Achilles tendonitis is an injury that occurs when your Achilles tendon -- the large band of tissues connecting the muscles in the back of your lower leg to your heel bone -- becomes inflamed or irritated. The signs and symptoms of Achilles tendonitis often develop gradually. You'll feel pain and stiffness in your Achilles, especially when you first get out of bed. The pain lessens as you warm up, and may even disappear as you continue running. Once you stop, the pain returns and may feel even worse. You may also notice a crackling or creaking sound when you touch or move your Achilles tendon.
Diagnosis
If Achilles tendonitis is suspected, avoid any exercise or activity that causes the pain. It is advisable to see a doctor promptly so that an accurate diagnosis can be made and appropriate treatment recommended. The doctor will take a full medical history and will ask about the nature and duration of the symptoms. They will perform a physical examination of the affected area. Ultrasound scanning may be used to assess damage to the tendon or surrounding structures. Occasionally MRI (magnetic resonance imaging) may be recommended. The symptoms of Achilles tendonitis are often similar to symptoms of other conditions such as partial Achilles tendon rupture and heel bursitis. This can make diagnosis difficult and a referral to an orthopaedic specialist may be required in order for an accurate diagnosis to be made.
Nonsurgical Treatment
With proper care for the area, the pain in the tendon should lessen over three weeks, but it should be noted that the healing of the area continues and doesn't even peak until at least six weeks following the initial injury. This is due to scar tissue formation, which initially acts like the glue to bond the tissue back together. Scar tissue will continue to form past six weeks in some cases and as long as a year in severe cases. After 6 months this condition is considered chronic and much more difficult to treat. The initial approach to treating Achilles tendonitis is to support and protect the tendons by bracing any areas of the tendon that are being pulled on during use. It is important to loosen up the tendon, lessen the pain, and minimize any inflammation.

Surgical Treatment
Most people will improve with simple measures or physiotherapy. A small number continue to have major problems which interfere with their lifestyle. In this situation an operation may be considered. If an operation is being considered, the surgeon will interview you and examine you again and may want you to have further treatment before making a decision about an operation. Before undergoing Achilles tendonitis surgery, London based patients, and those who can travel, will be advised to undergo a scan, which will reveal whether there is a problem in the tendon which can be corrected by surgery. Patients will also have the opportunity to ask any questions and raise any concerns that they may have, so that they can proceed with the treatment with peace of mind.
Prevention
To lower your risk of Achilles tendonitis, stretch your calf muscles. Stretching at the beginning of each day will improve your agility and make you less prone to injury. You should also try to stretch both before and after workouts. To stretch your Achilles, stand with a straight leg, and lean forward as you keep your heel on the ground. If this is painful, be sure to check with a doctor. It is always a good idea to talk to your doctor before starting a new exercise routine. Whenever you begin a new fitness regimen, it is a good idea to set incremental goals. Gradually intensifying your physical activity is less likely to cause injury. Limiting sudden movements that jolt the heels and calves also helps to reduce the risk of Achilles tendonitis. Try combining both high- and low-impact exercises in your workouts to reduce stress on the tendon. For example, playing basketball can be combined with swimming. It doesn?t matter if you?re walking, running, or just hanging out. To decrease pressure on your calves and Achilles tendon, it?s important to always wear the right shoes. That means choosing shoes with proper cushioning and arch support. If you?ve worn a pair of shoes for a long time, consider replacing them or using arch supports. Some women feel pain in the Achilles tendon when switching from high heels to flats. Daily wearing of high heels can both tighten and shorten the Achilles tendon. Wearing flats causes additional bending in the foot. This can be painful for the high-heel wearer who is not accustomed to the resulting flexion. One effective strategy is to reduce the heel size of shoes gradually. This allows the tendon to slowly stretch and increase its range of motion.
What Brings About Heel Discomfort To Appear

Overview
The Plantar Fascia is a strong ligament-like structure under the arch of the foot that runs from the heel bone to the ball of the foot. If we could see it in isolation it has a triangular shape when looked at from underneath but has a curved shape when looked at from the side - much like a sail boat’s sail billowing in the wind. The most functional piece is from the front-bottom-inside area of the heel bone (calcaneous) to the joint of the big toe (hallux) and this is where the majority of stress of walking (and running and jumping) is taken by the fascia. How your plantar fascia reacts to and recovers from this stress is what determines the extent and nature of your plantar fasciitis.
Causes
Plantar fasciitis most commonly occurs due to repetitive or prolonged activities placing strain on the plantar fascia. It is often seen in runners, or dancers and gymnasts who perform regular activities involving end of range foot and ankle movements. It may also occur in patients who walk excessively, especially up hills or on uneven surfaces. Older patients who spend a lot of time on their feet may also develop the condition. Plantar fasciitis frequently occurs in association with calf muscle tightness, inappropriate footwear, or biomechanical abnormalities, such as excessive pronation (flat feet) or supination (high arches). Occasionally the condition may occur suddenly due to a high force going through the plantar fascia beyond what it can withstand. This may be due to activities such as a sudden acceleration or a forceful jump.
Symptoms
Symptoms of plantar fasciitis include pain in the heel of the foot. Some people complain of a sharp stabbing pain especially with walking. Others describe the pain as a dull ache after prolonged standing. The pain of plantar fasciitis is often worst in the morning or following activity.
Diagnosis
After you describe your symptoms and discuss your concerns, your doctor will examine your foot. Your doctor will look for these signs. A high arch, an area of maximum tenderness on the bottom of your foot, just in front of your heel bone. Pain that gets worse when you flex your foot and the doctor pushes on the plantar fascia. The pain improves when you point your toes down. Limited "up" motion of your ankle. Your doctor may order imaging tests to help make sure your heel pain is caused by plantar fasciitis and not another problem. X-rays provide clear images of bones. They are useful in ruling out other causes of heel pain, such as fractures or arthritis. Heel spurs can be seen on an x-ray. Other imaging tests, such as magnetic resonance imaging (MRI) and ultrasound, are not routinely used to diagnose plantar fasciitis. They are rarely ordered. An MRI scan may be used if the heel pain is not relieved by initial treatment methods.
Non Surgical Treatment
No single treatment works best for everyone with plantar fasciitis. But there are many things you can try to help your foot get better. Give your feet a rest. Cut back on activities that make your foot hurt. Try not to walk or run on hard surfaces. To reduce pain and swelling, try putting ice on your heel. Or take an over-the-counter pain reliever like ibuprofen (such as Advil or Motrin) or naproxen (such as Aleve). Do toe stretches , calf stretches and towel stretches several times a day, especially when you first get up in the morning. (For towel stretches, you pull on both ends of a rolled towel that you place under the ball of your foot.) Get a new pair of shoes. Pick shoes with good arch support and a cushioned sole. Or try heel cups or shoe inserts ( orthotics ). Use them in both shoes, even if only one foot hurts. If these treatments do not help, your doctor may recommend splints that you wear at night, shots of medicine (such as a steroid ) in your heel, or other treatments. You probably will not need surgery. Doctors only suggest it for people who still have pain after trying other treatments for 6 to 12 months.

Surgical Treatment
Surgery may be considered in very difficult cases. Surgery is usually only advised if your pain has not eased after 12 months despite other treatments. The operation involves separating your plantar fascia from where it connects to the bone; this is called a plantar fascia release. It may also involve removal of a spur on the calcaneum if one is present. Surgery is not always successful. It can cause complications in some people so it should be considered as a last resort. Complications may include infection, increased pain, injury to nearby nerves, or rupture of the plantar fascia.